The Health Innovation Network polypharmacy programme aims to support local systems and primary care to identify patients at potential risk of harm and support better conversations about medicines by promoting shared decision-making, where clinicians and patients are equal partners in agreeing which medicines are important to treatment and life goals.
Access our Polypharmacy toolkit resources (one-time registration required for access to all HIW toolkits).
Why is this work important?
Over one million people in England take ten or more medicines for their long-term conditions.
As patients live longer with multiple long term conditions, physiological reserves to cope with taking so many medicines are reduced. What might have been an appropriate medicine in our fifties may be putting us at risk from harm in our eighties.
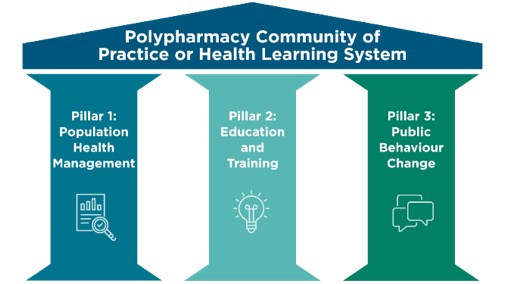
The three pillars of the polypharmacy programme have been developed to reflect our areas of focus.
Pillar 1: Popular Health Management
Using data (NHSBSA Polypharmacy Comparators) in primary care network areas to understand risks and identify patients for prioritisation for a structured medication review (SMR).
Pillar 2: Education and Training
Running local Polypharmacy Action Learning Sets (ALS) to upskill the primary care workforce to be more confident about stopping unnecessary medicines.
We created the polypharmacy masterclass series to allow a deeper dive into therapeutic topics highlighted by clinicians attending the Polypharmacy ALS. Check out our events page for details of upcoming masterclasses.
You can access more resources from the Polypharmacy toolkit (one-time registration required).
Pillar 3: Public Behaviour Change
Work from Scotland, Ireland and Northern Ireland has demonstrated savings not only in the drugs budget (from stopping inappropriate prescribing) but also in wider healthcare utility costs.
However, it is important that patients understand what an SMR is and its purpose. Evidence has shown that we need to do more to support patients to understand and make the most of their review.
Working together with the Health Innovation Network Polypharmacy Programme, Health Innovation Wessex has supported six primary care networks to help seldom heard communities access SMRs.
This project builds on work completed across the Health Innovation Network to use evidence-based materials to invite and support patients to get the most from their SMR. The project has focused on patients living in more deprived areas where studies in Nottingham and Manchester have started to show some important improvements.
Pragmatic Prescribing Guidance to reduce harm for older people with moderate to severe frailty from the British Geriatric Society (BGS)
This has been developed by geriatricians, GPs, pharmacists plus others and has been endorsed by NICE.
The guidance covers some common long-term conditions and supports prescribers in understanding the risks of harm in older people with moderate and severe frailty.
This publication highlights the importance of thinking carefully about the risks and benefits of medicines in this vulnerable patient group, where the evidence base may not be particularly robust.
This guidance is a much-needed resource in tackling the issue of problematic polypharmacy.