The issue:
Health Innovation Wessex was commissioned to support the Maternity and Neonatal (MatNeo) Safety Improvement Programme (SIP) preterm optimisation quality improvement activity, in conjunction with the South East Leadership Academy (SELA), Health Education England (HEE) and the Southampton, Hampshire, Isle of Wight and Portsmouth (SHIP) Local Maternity and Neonatal System (LMNS).
Four trusts received the coaching: Hampshire Hospitals NHS Foundation Trust, University Hospital Southampton NHS Foundation Trust, Portsmouth Hospitals University NHS Trust and Isle of Wight NHS Trust.
What we did:
Following a procurement process, coaching was provided by Rebekah Giffney Consulting Ltd between December 2022 and November 2023, to support the optimisation and stabilisation pathway through enhanced perinatal team working.
The project provided the four MatNeo teams with coaching focusing on culture, behaviours, and outcomes to help embed positive working practices and optimise patient care.
The coaching intervention was designed to enable teams to become high functioning, improving their communication, psychological safety and the effectiveness of the quality improvement work and outcomes. It was designed to identify individual and collective needs to facilitate personal growth and was tailored flexibly to support each person and the team.
What impact did it have?
An evaluation of the coaching intervention, undertaken by the Health Innovation Wessex Insight team, focused on the acceptability and impact of the coaching intervention across the four different maternity and neonatal units.
The evaluation aimed to review whether the coaching intervention worked to change organisational culture. To evaluate, two surveys (Psychological Safety Index and G3 Team Working assessment) and one set of interviews were undertaken.
The evaluation sought to answer the following questions:
1. How acceptable was the team coaching programme?
2. Was the flexible / tailored training experience useful?
3. Do participants feel their own behaviour has changed because of the coaching?
4. Do participants feel their team has changed because of the coaching?
5. Are there any wider impacts from participation in the coaching programme?
6. Have any changes in team working been sustained?
Programme highlights and key statistics
1. Psychological Safety Index (PSI)
Thirty-three staff completed the pre-coaching PSI and twenty-seven staff completed the post-coaching PSI.
All units saw a positive change in their psychological safety score, which indicated the coaching was valuable regardless of the starting position of the maternity and neonatal unit. Unit 1 reported a more significant improvement compared to other units.
The training appeared to have less impact on Unit 4. Contextual reasons of the broad geographical location of staff and staff turnover during the coaching intervention help to explain this.
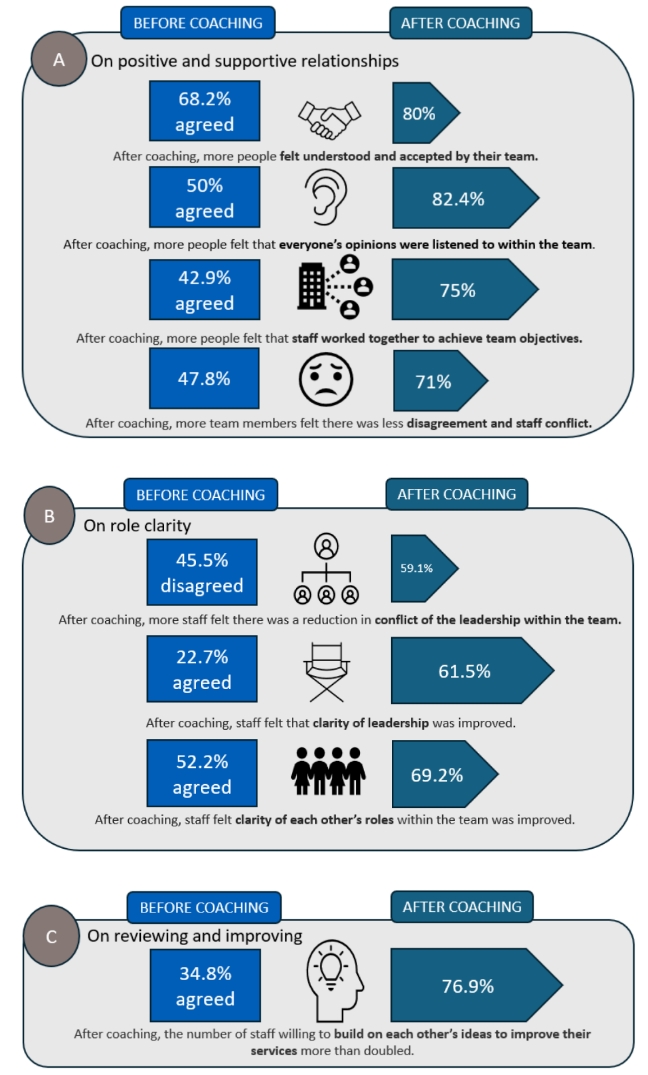
2. G3 Team Working Assessment
Taken from the NHS Culture and Leadership Programme, the G3 Team Working Assessment is a survey designed to assess the effectiveness of a team. It is designed as a five-point Likert scale, ranging from strongly disagree to strongly agree. A sixty-four percent response rate was obtained.
Summary of actions
The full evaluation report has been shared with SHIP LMNS and Rebekah Giffney Consulting Ltd. The programme and evaluation have been shared within the Health Innovation Network, NHS England South East and South West regional teams, and neighbouring local maternity and neonatal systems. As part of the 2024/25 Patient Safety Collaborative commission for Perinatal Culture and Leadership support, the programme and evaluation will also be shared with the quadrumvirate teams (leadership teams within maternity that include midwifery, obstetric, neonatal and operational management) within each Wessex trust.
As part of the project, each trust chose an element of the preterm optimisation bundle to focus quality improvement initiatives as a perinatal team. The impact of the coaching programme on the focused elements was out of scope for the initial evaluation. However, this is being locally and regionally monitored and an updated case study will be published in due course.
Recommendations
To maintain momentum after the project coaching sessions end, dedicated time is needed for the perinatal optimisation teams to continue to network and build on the learning. This has proved challenging within some units.
With the improvement in perinatal team working, there is now a need to apply the learning from the coaching programme, beyond the focused element, to all nine elements of the optimisation bundle.
The clinical teams involved in the programme recognise the benefits of having funded multidisciplinary team posts rather than one speciality role (mirroring the NHSE quadrumvirate culture work for senior leaders - where midwifery, obstetric, neonatal and operations have joint responsibility for leading maternity change).
Strategic alignment
This piece of work links to our patient safety commission for preterm optimisation, a key safety priority in the NHS patient safety strategy. It also supports workforce as a cross-cutting theme.