Audit findings:
- 84% of adult trauma patients were discharged on opioids
- More than 32% remained on an opioid at six weeks
- 22% continued to take opioids at six months.
Patients who might have been taking opioids previously for long term chronic pain were removed from the audit and a further review was undertaken of patients who were newly-commenced on opioids (16% of sample).
At six weeks:
- 27% of these newly-commenced (opioid-naïve) patients remained on opioids
- 16% were still receiving opioids at six months post discharge.
Discharge summaries were reviewed for those opioid-naïve patients to review the advice provided for both patient and clinician in primary care.
The audit found:
- Of 37 elective surgical patients, 35 were prescribed one opioid. The remaining two patients were prescribed two opioids
- 81.5% of opioid-naïve patients were given no guidance at all on discharge
- 77.6% of patients had no information entered on the GP advice section of the discharge summary.
Impact of the audit
The Trust was keen to address the audit findings, and the pain service team proposed to develop a compulsory section on the discharge summary for any patients newly initiated on an opioid as a solution to the audit findings.
The request was positively received but the Trust queried if this intervention would stop the inappropriate continuation of the opioid for longer than was intended.
The pain team needed to understand what primary care colleagues would find beneficial in a discharge summary to prevent inappropriate continuation of opioids and raised the issue at the Wessex Opioid Working Group.
Health Innovation Wessex offered to host a workshop to explore and document the challenges faced by primary care colleagues in relation to patients prescribed an opioid on discharge and to explore suggestions to address the audit findings.
The role of Health Innovation Wessex
Health Innovation Wessex convened a Wessex-wide, opioid discharge workshop. We invited primary care clinicians (GPs and pharmacists) to discuss the following questions:
- What are the challenges you face when patients come out of hospital?
- What happens to increase harm and is difficult for patients?
- What is frustrating for GPs and [primary care] practices?
- What could we do to make this safer?
- How can we improve patient experience?
- What could happen to help?
A full report of the discussions was produced and shared with UHS. This resulted in the Trust agreeing to develop an opioid e-Discharge protocol.
In January 2024, the Wessex Opioid Working Group and UHS clinicians co-produced the electronic discharge summary wording.
This will include the following compulsory fields for ALL patients prescribed an opioid on discharge:
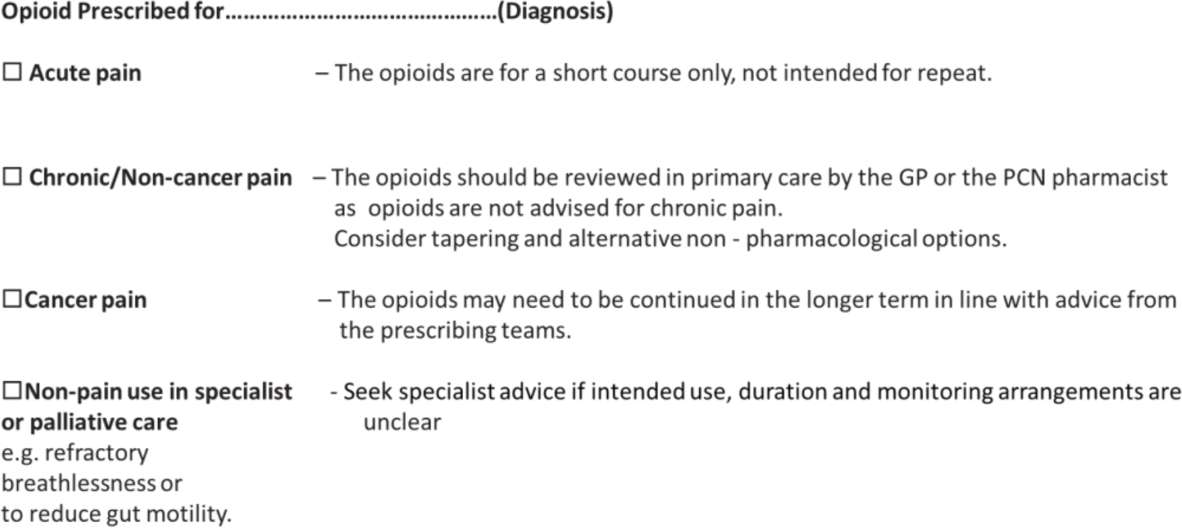
Next steps
Following approval from the Trust’s Drugs Committee and discussion at the digital programme meeting, the new opioid e-discharge summary template has been developed and due to go live in early 2025. Health Innovation Wessex are currently developing the evaluation process and plan to facilitate adoption of the opioid e-discharge protocol across other trusts in Hampshire, the Isle of Wight, and Dorset via our existing Wessex Opioid Working Group network.
What were the learning points?
What lessons does the initiative hold for the organisation and for others?
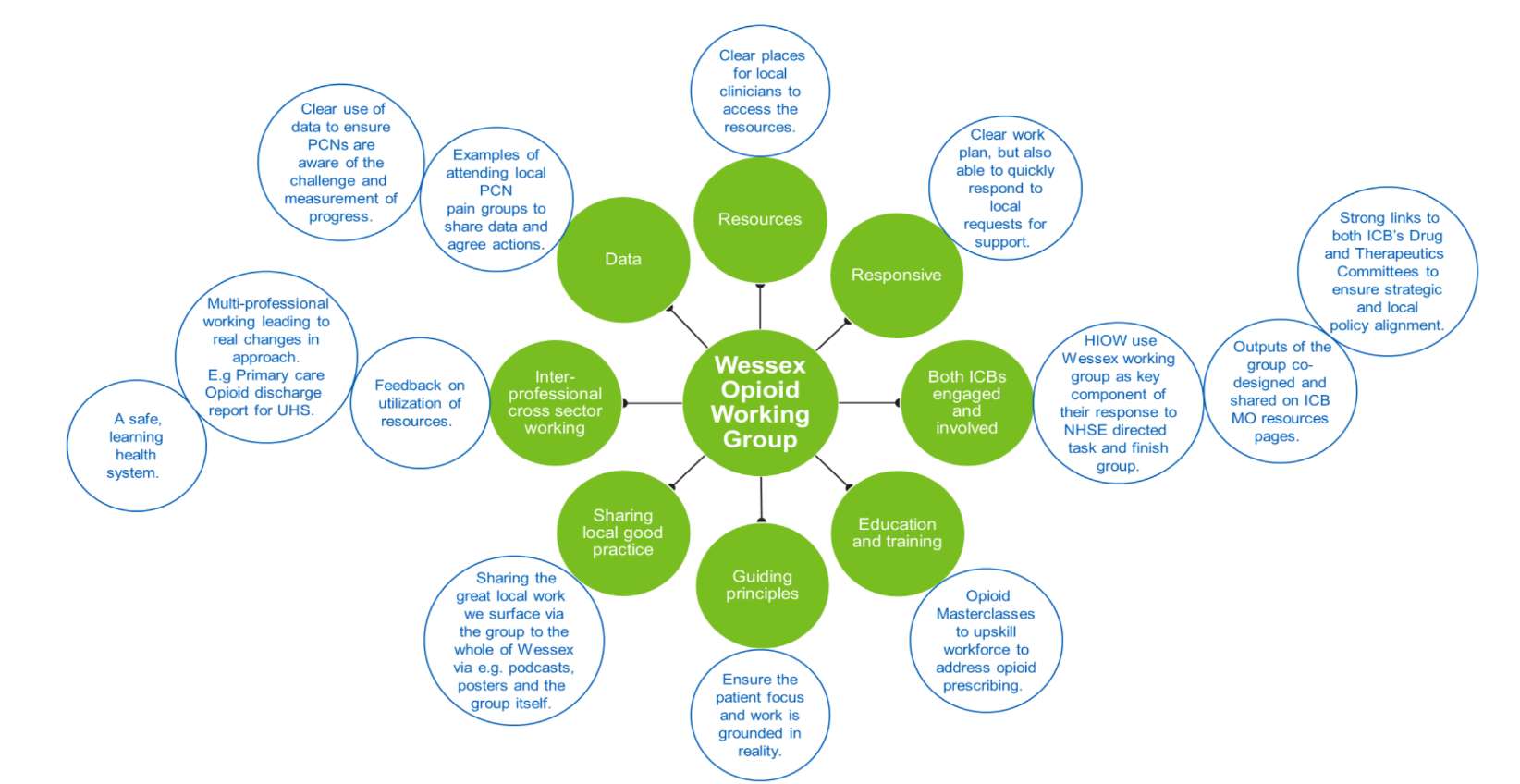
- A cross-sector, multidisciplinary network or working group is vital to resolve complex issues such as opioid prescribing across the interface between primary and secondary care.
- Getting clinicians together to discuss focused topics can foster better working relations and help resolve issues that individual sectors may not realise are impacting negatively on patient safety.
- Having a working group of experienced, cross-sector clinicians who understand the roots of a problem can be very helpful in resolving challenges such as how to word an e-discharge summary. Collaboration is key, especially for complex, multisector problems such as the overuse of opioid analgesics.
Annex 1.
The Wessex opioid network was formed in June 2021 and has been integral to the success of the project, bringing together clinicians from primary and secondary care.